Inventing a new, alternative, modernised mental healthcare system
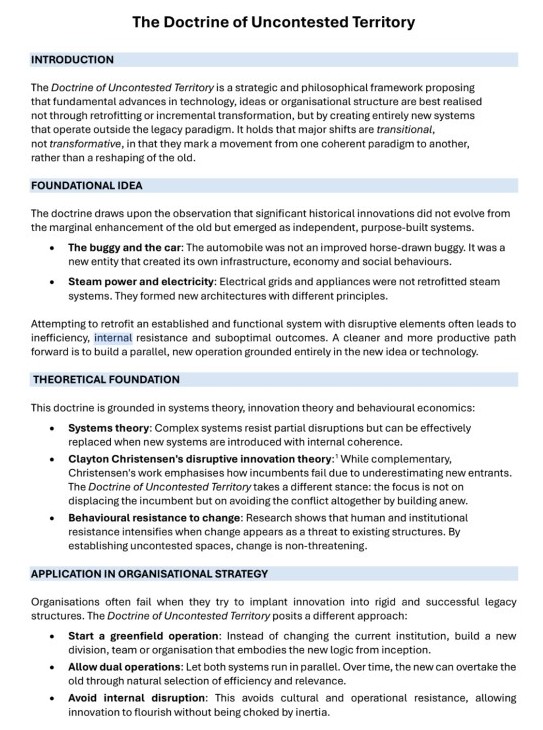
We need to embrace the radical core strategy that Peter Fritz’s Doctrine of Uncontested Territory has highlighted in order to solve the problem of our collapsing Australian health care system.
In my role as Chair of the RANZCP Section of Private Practice Psychiatry (at the Faculty of Adult Psychiatry 2025 Conference in the Barrossa Valley, Adelaide), I convened a 'workforce workshop', on 29 June 2025. Ex-AMA President and Avant Chief Medical Officer, Dr Steve Robson, was invited to deliver a keynote presentation to consider the status of our mental health system. Health editor of The Australian, Natasha Robinson, also participated in the vibrant discussion with 170 psychiatrists who attended.
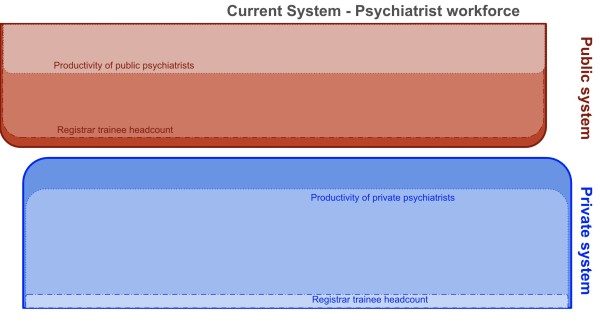
We commiserated about how the health system does not meet the present needs of mental healthcare and that, in its current shape, it cannot meet the growing future needs of the community. Steve, Natasha, Dr Jeff Looi and I had published in the media how the system was failing the most needy and is unfit for purpose.


We have a healthcare system that needs to be modernised. The Doctrine of Uncontested Territory asserts that the solution needs to be found through “transformative innovation”. Emerging technologies, novel models and new systems need to be used to markedly outperform the old, outdated, failing system...through “transcendence”.
But incorporating new technologies into an old system is doomed to failure. That's because the old (present) system is in survival mode - in a defensive ('fight or flight') mode of operation, with gross inefficiencies (overridden with bureaucrats using bureaucratic unworkable solutions). A system like this resists new, more efficient, contrary methods.The Doctrine says: “Research shows that human and institutional resistance intensifies when change appears as a threat to existing structures. By establishing uncontested spaces, change is non-threatening.”
Politicians and bureaucrats have intuitively recognised principles of the Doctrine, as they have been pumping funds into alternative systems, other than the private and public - for example, to NGOs and insurance schemes such as the NDIS and private health insurers.
But these entities are bureacratic, self-serving, ideologically driven and short-term economically driven, so they lack innovation. They are flawed, band-aid options unable to meet the needs of the community. Furthermore, this approach has accelerated the demise of the public sector, which now focuses on nothing other than crisis care. And the private sector (which enables way more superior, effective and efficient healthcare, as it still largely allows doctor-patient decision making) has been isolated even further. This cas caused more fragmentation and frustration of consumers and their families, unable to navigate the fiefdoms and wasting time trying out inadequate models.
Instead of trying to reform the outdated systems by pumping more funds into them, we need an entirely alternative strategy. We need to invest funding into a new model/system/method that can perform more superiorly. The good news is that we now have the technological building blocks that we can use to assemble and create a new, alternative, productive, efficient, affordable, scalable healthcare system. This new system will augment traditional approaches, and markedly outperform the mishmash of current models.
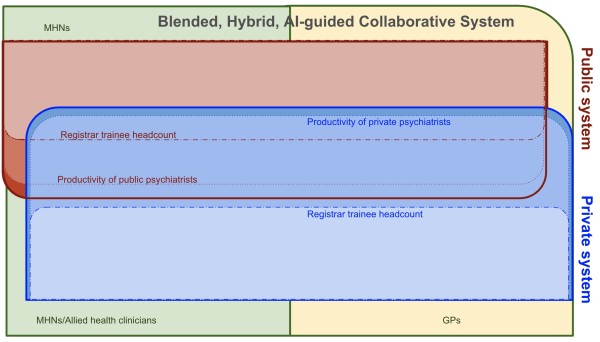
In line with the Doctrine, emerging technologies and new models of care can revolutionise the effectiveness, efficiencies and productivity of the mental healthcare workforce. For example, digital platforms enabling person-centred shared care and Artificial Intelligence can empower service developers to integrate and enhance the fragmented public, private, NGO and insurance sectors to create a blended, hybrid, AI-guided collaborative system:
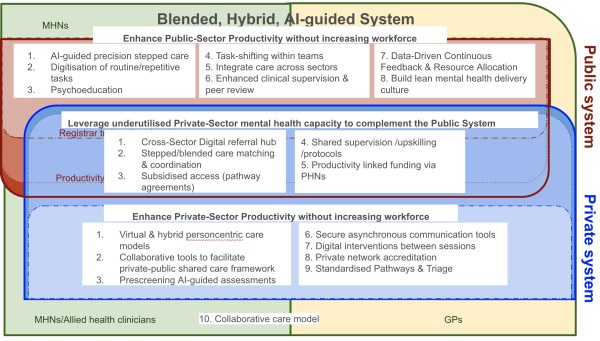
Collaborative care between these systems can be enhanced by technologies like MindSkiller®. With an eLearning program at its heart, the platform lays the foundation to a virtual clinical governance methodology to enable small numbers of psychiatrists to remotely manage substantial numbers of patients undertaking new interventions like TMS delivered by support staff. Upon that layer is a personalised suite of tools that enhances multidisciplinary team (MDT) care and person-centred inter-team coordination, whether the MDTs are virtual or in-person.
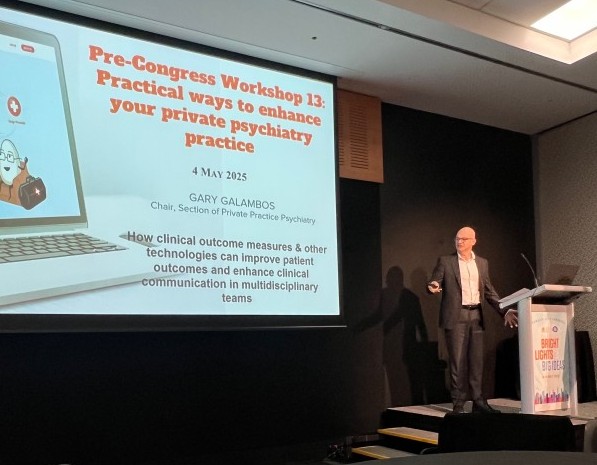
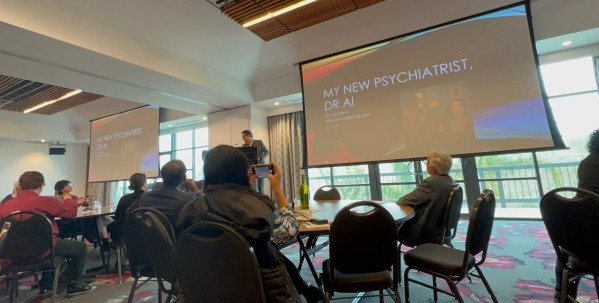
This technology was showcased to psychiatrists at the RANZCP Annual Congress at the Gold Coast in May 2025 in a Section of Private Practice workshop, an Outcome Measurement symposium and a symposium chaired by A/Prof Jeff Looi exploring the impacts of new technologies on the private practice system, followed by a PsychMatters podcast with RANZCP Board member Dr Michelle Atchison, Jeff and myself (not published yet).


A growing number of clinicians are now focused on developing powerful emerging technologies, such as AI-driven clinical tools, asynchronous psychiatric assessment and mental health utility platforms to support private sector research and development.
The future of psychiatry is here - with translational interventions (e.g. MRI-guided TMS, VR and digital medtech) and AI-guided behavioural activation and coaching tools ushering in a new era of advanced, precision, and personalised mental health care.
At the Faculty of Adult Psychiatry 2025 Conference , symposia lectures and workshops introduced psychiatrist attendees to emerging technologies such as AI-guided documerntation and formulation, VR-delivered AI-guided positive emotion activation, and AI-guided psychometric assessment.


I was delighted that my neurologist 'twin' "psychointerventionalist" Dr Stephane Verhaeghe, who is collaborating with me at Uspace Young Adult Mental Health Service at St Vincent's Private Hospital Sydney to progress the R&D work within our 'mental health innovation incubator' I've established there, enjoyed outlining to a packed room of psychiatrists the groundbreaking work he has been doing with Brain Vector using VR-delivered AI-guided positive emotion activation, at the SPPP 'future technology symposium', which complemented the 'AI symposium' preceeding it.

I enjoyed watching the faces of my colleagues when an AI companion skillfully interviewed a mock patient who only partially complied with the questions exploring DSM-5 ADHD criteria based on the DIVA-5 questionnaire, overseen by a mock psychiatrist collaborating with a mock GP delivering person-centred shared care.

A symposum was also conducted at the FAPC 2025 considering how we are going to fund the training of psychiatrists in private practice - to ensure we have a fit, broadly skilled psychiatrist workforce, trained to deliver hybrid technology-enhanced models of care of the future. Three funding models were considered (private-public partnership, self-funded, and applying a version of the existing GP supervision funding model to private practice psychiatrists) in a symposium about transforming the way we train psychiatry registrars, enabling them to undertake psychiatric training in private practices across Australia and NZ.


As the Doctrine says, we need emerging technologies and novel models to create new systems to transform healthcare.Two original pilot projects are ready for implementation:
1. An education/training and supervision/mentorship program for GPs to collaborate with psychiatrists to enhance ADHD mental health care in NSW.
2. A private sector training program that will enable psychiatry registrars to complement their colleagues in both the public and private sectors.

I am very excited that my colleagues have responded so positively to the multi-faceted work I am doing to develop and incorporate new and emerging technologies into clinical settings using best practice person-centred share care models to revolutionise psychiatry.
The time has arrived for us to take a lead role. We need to provide clinical governance to ensure these technologies are used in a helpful and safe manner. The collaborations are growing.
We need passion, courage and grit to invent a new, alternative, modernised mental health system.